I have one leg longer than the other. My right leg is 9mm shorter than my left. This is called leg length inequality, also known as leg length deficiency, leg length insufficiency, or short leg.
This was diagnosed reliably from an x-ray while I attended Chiropractic University over two decades ago.
X-Ray is the only reliable means for measuring leg length inequality. As a result of my short leg, I have associated lumbar scoliosis and a history of disc degeneration in this region of my spine. Ugh!
Personally and clinically – after years of treating patients with leg length inequality, having regular manual adjustments, and wearing a heel lift – I believe my chronic back pain was primarily associated and caused by my leg length asymmetry. The medical research, however, may contradict my self-diagnosis.
Leg Length Inequality
Before the 1970s, leg-length inequality (LLI) data was unreliable in leg length measurement from x-ray.
A review by Gary Knutson – published in 2005 in Chiropractic and Osteopathy, used LLI data from 1970-2005. All the studies reviewed were selected because they used accurate radiological methods to determine anatomic LLI. Those that failed to use accurate radiological methods were excluded from his review.
Leg-length inequality (LLI) is a topic that has been examined extensively. However, several questions have mainly remained unanswered regarding leg-length inequality and include:
How common is LLI?
What is the average amount of LLI?
What are the effects of LLI?
The purpose of Knutson’s review was to highlight current research to answer these questions.
Prevalence of Leg-Length Inequality
Several studies using precise radiographic method data were combined, giving a subject size of 573, with an LLI range of 0–20 mm. The mean or average LLI was 5.21 mm. What’s interesting is that most Chiropractors who treat LLI start using heel lifts at 5mm. It seems that science backs this decision up.
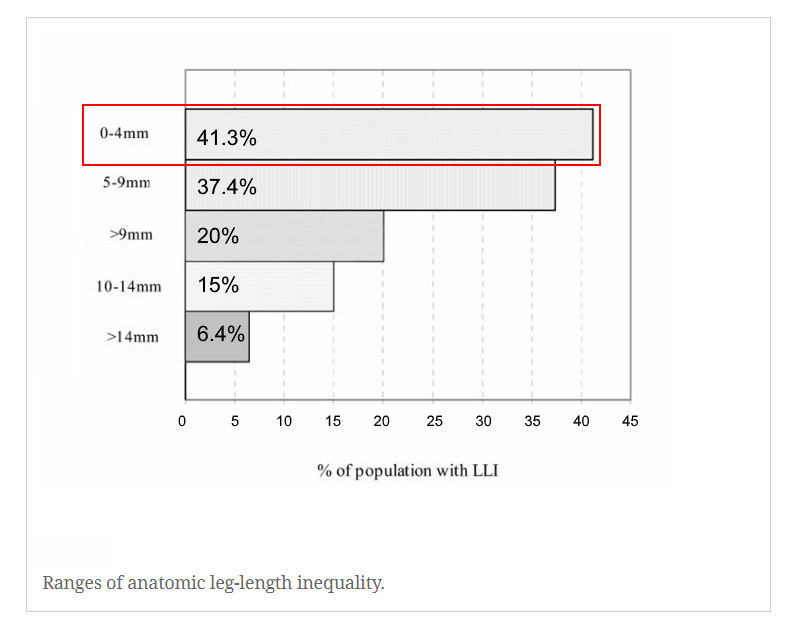
It seems a much higher percentage of the population has LLI closer to 5 mm.
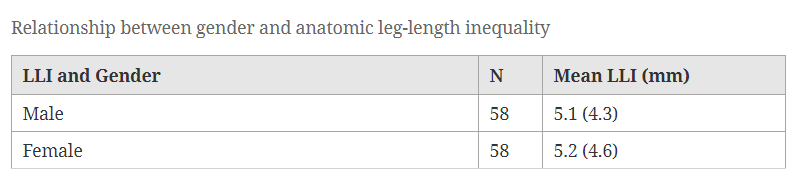
Four of the studies reviewed by Knutson measured subjects by gender. No difference between males and females was found, suggesting that gender plays little role in LLI.
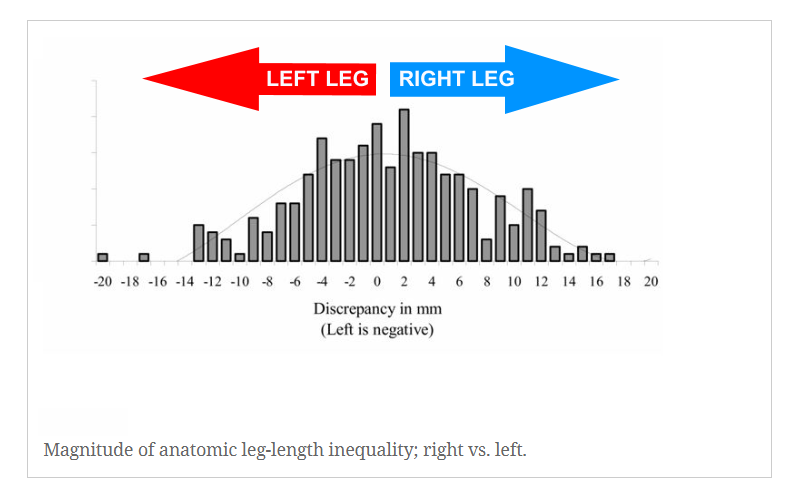
The data also demonstrates no preference for the left or right leg, which fascinates me. Many musculoskeletal diagnoses have a one-sided inclination. For example, thoracic scoliosis to the right makes up 85-90% of all adolescent scoliosis; stroke more frequently affects the left side of the brain, and 90% of the world’s population is right-handed!
Seven of Knutson’s studies identified subjects with LLI as symptomatic (subjects = 347) or asymptomatic (subjects = 165). Symptoms included knee and hip problems and low back pain (mainly within the last 12 months).
I find it amazing that there is no statistical difference between these two groups, suggesting that the average LLI is not correlated to symptomatic problems, like low back pain.
Note: There will always be individual exceptions. Just because research fails to show a correlation between leg length inequality and back pain, does not mean a relationship doesn’t exist.
Effects of LLI
The most common effect of anatomic LLI is rotation (twist) of the pelvis – often referred to as pelvic torsion. Knutson explains that the body’s weight in the pelvis (on the short leg side) induces a downward force towards the feet in the standing position. With asymmetry of the leg-lengths, the pelvis, being pushed down on the femoral head (hip), must rotate or torsion.
So if you have a left short leg, it is likely that your pelvis drops down to the left and twists right or away from the short leg side. This is how we measure it on x-ray:
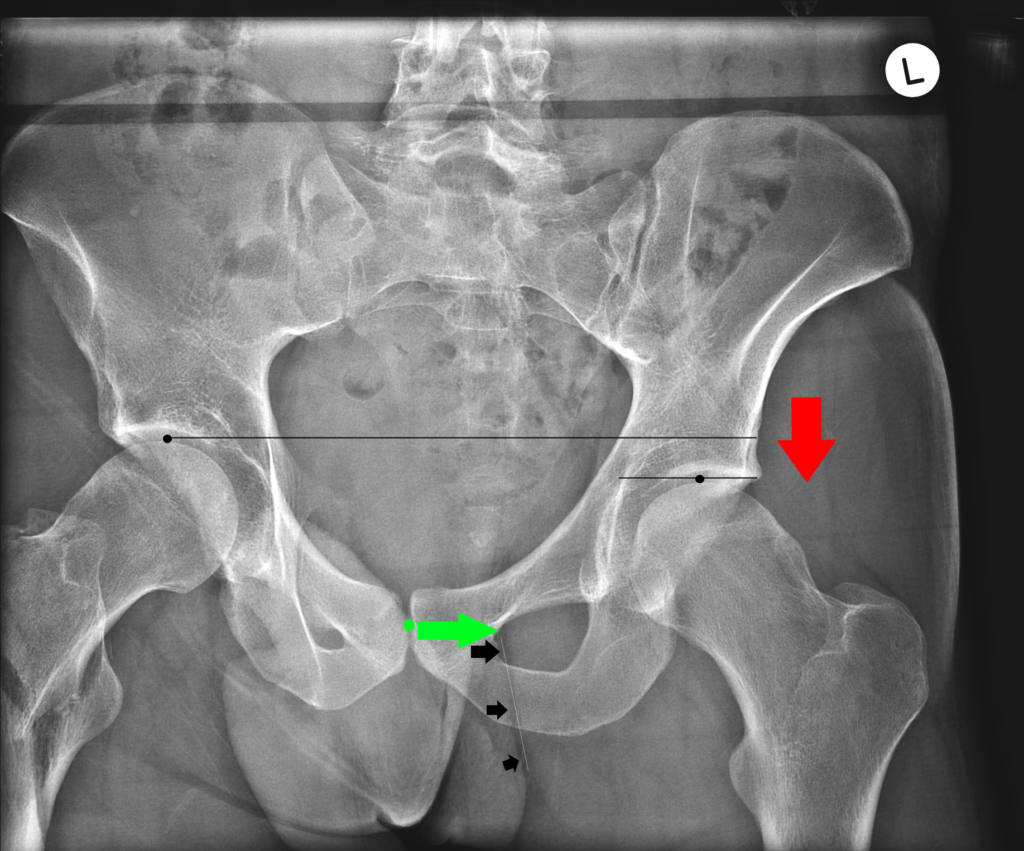
Here you can see a very clear LLI on the left side. The result is a downward force toward the left femoral head of the hip, with a right torsion or twists through the pelvis. This would mean that your pubic bone (green dot) would be visualized to the right of your gluteal fold (white dotted line) on x-ray.
The amount of pelvic torsion from this left LLI is measured by the distance between the pubic symphysis joint and the gluteal fold, illustrated by the green arrow.
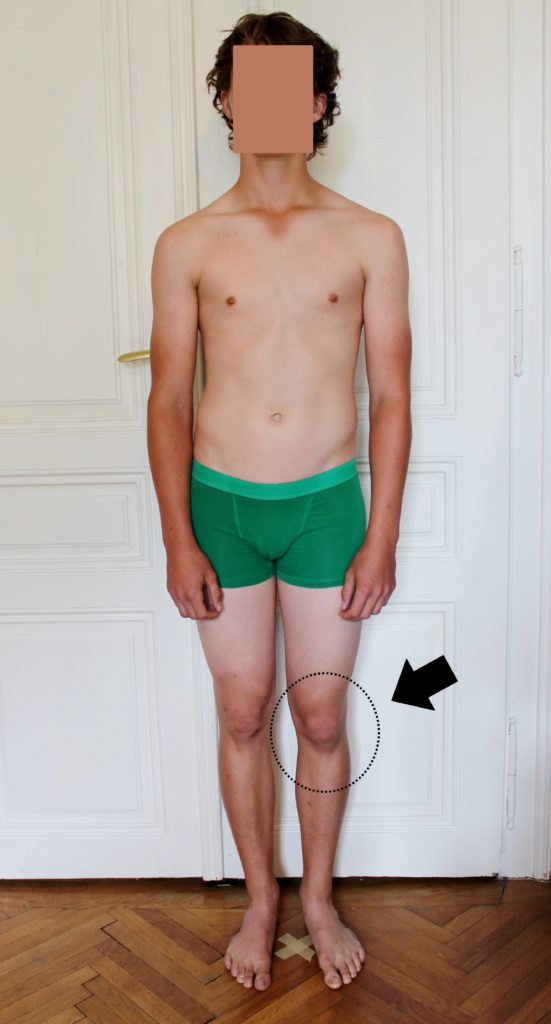
With more significant amounts of leg-length inequality (greater than 22mm), subjects in this study developed knee flexion on the long leg side. This is the body’s clever way of attempting to level up the pelvis.
Other effects of LLI and pelvic torsion demonstrated in the research literature include postural scoliosis, wedging of the 5th lumbar vertebra, and bone traction spurs (osteoarthritis).
Clinical significance
Knutson’s research attempted to quantify what ranges of LLI are clinically significant, associated with back pain, injury, muscle strength asymmetry, or other physiologic changes.
Chronic low back pain and LLI
Chronic low back pain affects about 21% of the population. One would expect this percentage to be higher if LLI caused low back pain, given that 50% of the population has an LLI of 5.2 mm or more.
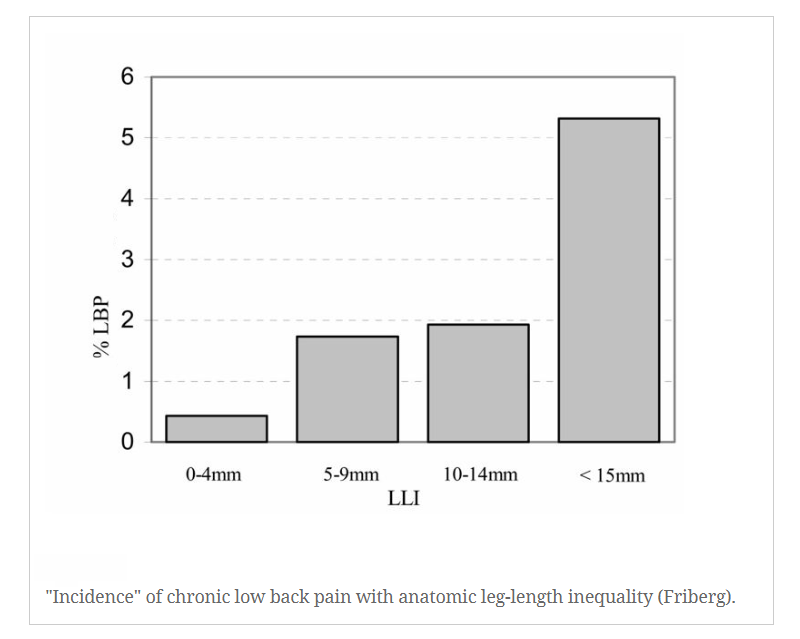
As you can see, the correlation between LLI and chronic low back pain becomes demonstrable when LLI is above 15 mm.
In this study, Dr. Oro Friberg notes that relatively small amounts of LLI may only be clinically significant relative to conditions such as prolonged standing or gait, such as daily work, marathon runners, military training, and sporting activities.
In this study, Gofton and Trueman found a strong association between LLI and osteoarthritis (OA) on the side of the anatomically longer leg. I often explain it to my students in this way: The more extended leg hip joint gets impacted with increased load, as forces are pushing upwards, much as forces are pushing downward (with gravity) on the short leg side.
In their study, few subjects were aware of any difference in leg length. However, the authors acknowledge that many with LLI fail to develop this condition, suggesting that other factors may also be important.
LLI conclusion
In summary, childhood-onset leg-length inequality appears to have little clinical significance up to 20 mm. However, past the ~ 20 mm point, structural changes may cause compensatory muscular contractions.
The purpose of Knutson’s paper was to review the research regarding leg-length inequality, prevalence, mean magnitude or size, effects, and clinical significance.
The prevalence of leg length inequality seemed almost universal and was ninety percent of the population. However, the average magnitude of LLI was small and found to be 5.2 mm. Based on the research reviewed, small childhood-onset LLI under 20mm (under typical situations) does not seem clinically significant.
It seems the body is well able to compensate for minor LLI of up to 2cm. However, as a Posture Doctor who has spent years treating 100’s of people with LLI (including myself), I feel much more research is needed to convince me.
Until that time, I will continue to help those of you with LLI and your associated postural distortions; to bring your pelvis back towards a neutral orientation and decrease active muscular compensations through heel lifts, effective exercise programs, and manual treatment.
Further Resources: Scoliosis Exercises You Can Do From Home



