Suppose you’re over the age of 35 and have spent years either sitting behind a desk, driving, laboring or otherwise being very physically active. In that case, you might have a condition commonly called Flatback Syndrome.
What is Flatback Syndrome?
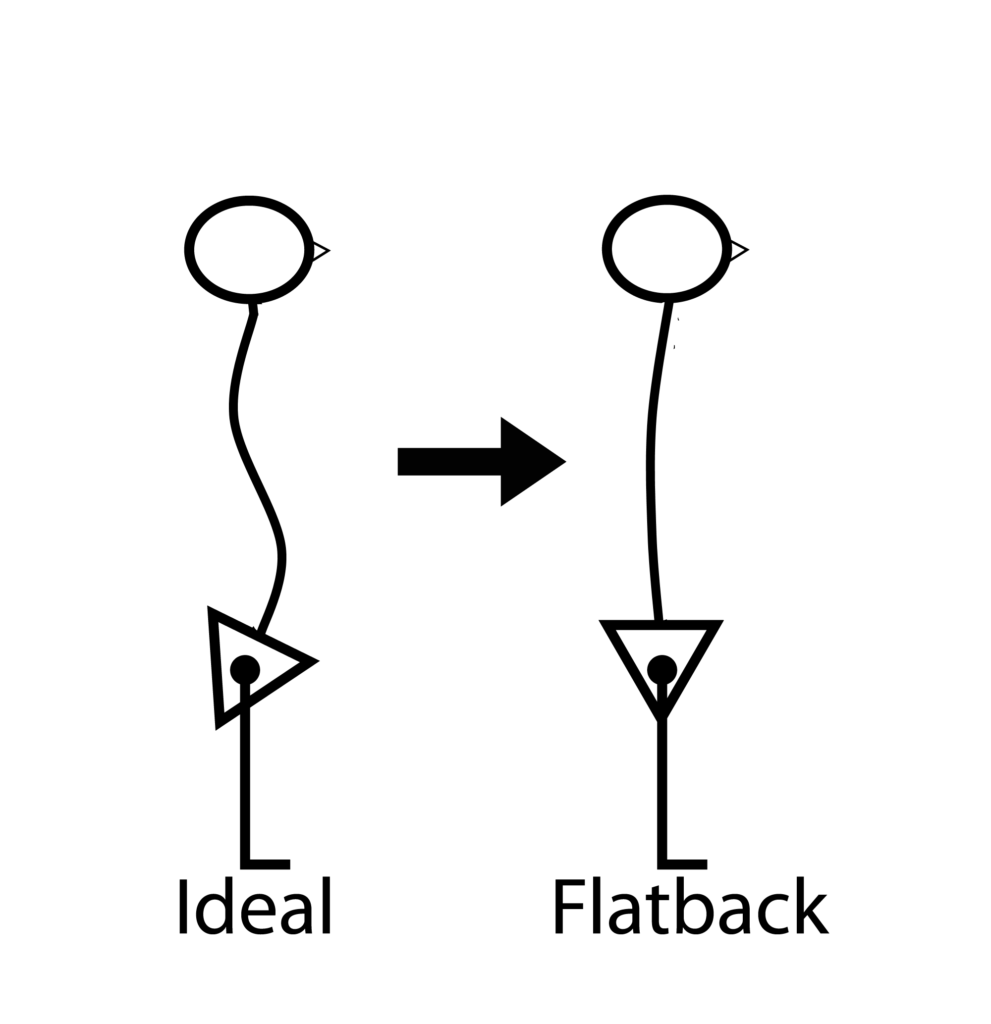
Flatback Syndrome is not a syndrome as such. Instead, I prefer to call it flatback posture or the correct medical term, alordosis.
Lumbar Lordosis is the normal inward curvature in the lower spine. “Alordosis” means “absence of lordosis” – the normal curvature isn’t present, and instead, the lower back is “flat.” The pelvis is usually tipped backward (posterior tilt), associated with or causing the normal spinal curve to flatten. This is Flatback Syndrome
Signs and Symptoms of Flatback Syndrome
- flat lower back curve
- forward head
- round shoulders
- low back pain is often described as ‘aching.’
- groin pain
- leg pain
- spinal stiffness, especially on waking
This list is only a guide. You may have many of the signs and symptoms listed, only a few or none of them. The list is to assist you in recognizing whether you have Flatback Syndrome.
What Causes Flatback Posture?
Incorrect Sitting
If you have spent years sitting incorrectly – sitting on your bottom muscles instead of sitting with your back aligned over your hips – you may have developed chronic muscular imbalances – short, tight abdominals, short, tight hamstrings, and weak hip flexors – pulling the pelvis into a tucked-under position (called posterior pelvis).

Slouch Sitting – copyright Posturo Global Ltd
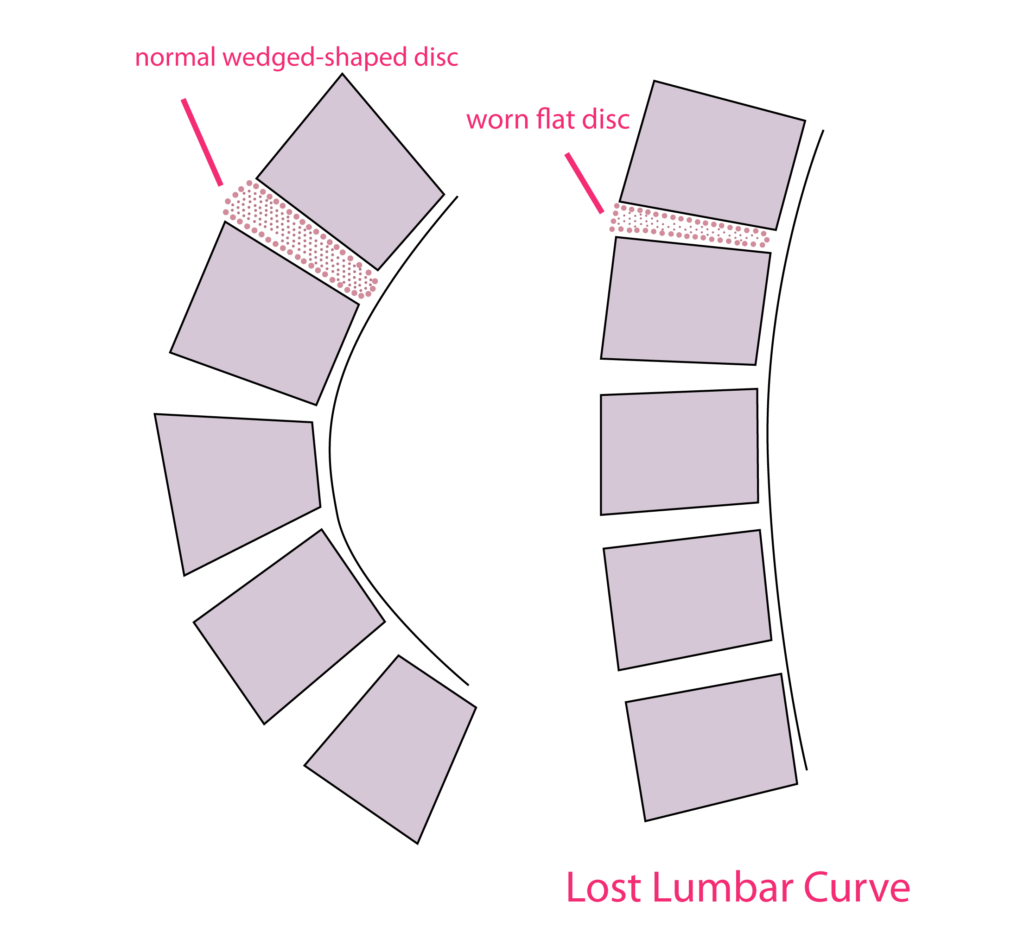
Disc Degeneration
Incorrect sitting and standing posture, poor nutrition, injuries, athleticism, and manual labor can lead to worn spinal discs and pain in a patient. In addition, the lower spinal discs should be wedged-shaped, which gives the lumbar region a healthy inward curve, known as lumbar lordosis.
Interesting: When people say, ‘I’ve got lordosis in my lumbar spine,’ what they usually mean is that they have hyperlordosis or sway back. The hyper suggests an increase to the normal lumbar curve. We should ideally all have lordosis in our lumbar spine.
If the lumbar curve is exaggerated, it is a hyperlordosis; if it is flat, it’s an alordosis or without a lordosis. So saying you have ‘lumbar lordosis’ is saying you are normal. That always makes me laugh – in a kind-hearted doc sort of way.
When our spinal discs degenerate, they lose their natural wedge shape, causing a reduction in natural lordosis. This may result in a flatback posture. It may also be common to see spinal curvature.
Herniated Disc
A herniated disc is just a severely degenerated disc, where the gelatinous, toothpaste-like material commonly found contained inside the disc has leaked through the outer cartilage rings. This also causes a loss of the natural wedge shape, which leads to a change in the normal lordotic curve.
Chronic Muscular Imbalance
Many muscles responsible for posture and body movement are found in “pairs.” One muscle (or group of muscles) moves a body part in one direction, while the paired muscle moves the same body part in the opposite direction. The two sides of such a pair are said to be “opposers” since the effort of one side opposes – works in the opposite direction to – the other side.
Both sides of a muscle pair’s efforts may also be exerted simultaneously (when sitting or standing relatively still) to provide the tension and support needed to hold a body part steady in a desired balanced position.
Further Resources: Balance Exercise for Beginners
When one of the muscles of a pair becomes stronger than its opposer, we say that the stronger one has become dominant. This is because dominant muscles tend to become short, tight, and over-aroused – or facilitated – neurologically. Conversely, the weaker opposing muscle becomes long and under-aroused or passive.
Although these muscular imbalances are reasonably predictable, individual differences do, of course, exist. Muscle imbalances commonly found in people with flatback posture include:
Dominant Short Muscles
- Abdominals
- Hip flexors
Passive Long Muscles
- Hamstrings
- Gluteals
Because posture and muscular imbalances affect how we move, problems in one area lead to other places. For example, flatback posture often contributes to round shoulders and forward head posture.
Other problems may result from the muscular imbalances found in flatback posture, including:
- Sciatic leg pain (from inflamed, bulging discs)
- Chronic lower back pain
- Acute lower back muscle spasms (often one-sided)
- Scoliosis
- Degenerative disc disease
- Deformity
It is not essential to know the exact cause of your flatback syndrome. Still, it suggests some daily posture exercise habit is needed to return mobility and optimal alignment to the spine. Spinal surgery correction or other surgical treatment is not ideal. However, surgery and physical therapy can help you, especially if you have a pinched nerve, neck pain, or other severe pain.
The patient’s objective is to restore good alignment by establishing healthy posture habits and daily routines. Good posture is a habit and one that you can learn to love. It also helps avoid spine surgery or other intrusive treatments for the spine.
After Thought – Best Ergonomic Tip
A fully upright posture (90°) is hard on the discs in your low back, so avoid buying the “perfect ergonomic chair” that keeps you bolt-upright. Research has shown that reclining at a 135° angle is the least damaging to our lumbar discs when seated.
Before you jump and adjust your seat angle, recognize that such a position is impractical for working at a computer. You’d be so far back, you’d be straining to reach the keyboard, and you’d almost certainly increase your forward head position.
It seems that 110-120° is about perfect for reducing any forward head posture that could occur if you incline the seat back any further. Therefore, I favor 120°, with lumbar back support.

In any event, do remember to keep your head back, nicely inline above your shoulders. Please don’t force it back; allow a gentle lengthening to lift your head back into alignment.
Review the chin tuck exercise for forward head posture if you are unsure.
Inclining your seat 5° downward at the front and using armrests can further reduce lumbar disc pressure.
Flat Back Syndrome – Diagnosis And Exercises
Flat back syndrome is a common and serious condition that affects millions of individuals around the world. According to recent studies, up to 25% of adults in the U.S. suffer from flat back syndrome, making it one of the most prevalent musculoskeletal problems experienced by Americans today. As physical therapists and physiotherapists who specialize in treating this condition, it’s our job to ensure those affected have access to accurate diagnosis and effective exercises for relieving their pain and improving their quality of life. In this article we’ll discuss exactly how flat back syndrome can be diagnosed as well as some simple yet powerful exercises designed specifically for managing its symptoms.
The effects of flat back syndrome are far-reaching, resulting in impaired mobility and reduced postural stability which can severely limit an individual’s ability to perform even basic everyday activities with ease. Fortunately though, if caught early enough there’re lots of things that can be done to prevent or reduce the progression of the condition – allowing sufferers to maintain an active lifestyle free from unnecessary discomfort or limitations.
It all starts with getting an accurate diagnosis so you know what kind of treatment plan needs to be put into place; then comes developing targeted exercises tailored towards strengthening key muscle groups involved. This means understanding how each exercise works within your body, knowing when they should be performed, and establishing a regular routine that will yield long term results over time. We hope this article provides useful insight regarding both aspects – helping readers diagnose and manage their own flat back syndrome safely and effectively!
Identification Of The Condition
Flat back syndrome is a spinal deformity that affects the lumbar spine, thoracic spine and/or sacrum. It can cause pain in these areas as well as reduced mobility. Symptoms may include stiffness, poor posture, difficulty standing or walking for long periods of time, fatigue, and trouble with activities such as sitting down or getting up from chairs. Common causes include degenerative disc disease, scoliosis, spondylolisthesis, spinal stenosis and trauma to the spine.
To diagnose flat back syndrome accurately requires careful evaluation by a physical therapist or physiotherapist experienced in treating this condition. During an assessment they will look at range of motion in the lumbar and thoracic regions; observe movement patterns; assess strength, flexibility and coordination; evaluate muscle tightness; review medical history; and perform palpation to check for tender points or restrictions in soft tissues throughout the area affected by the condition.. In addition, imaging tests such as x-rays and MRIs may be used to confirm diagnosis.
Once diagnosed with flat back syndrome appropriate exercises can help relieve symptoms while improving core stability, strengthening muscles around the spine, increasing range of motion and restoring balance between opposing muscle groups.
Causes Of Flatback Syndrome
Imagine a person standing upright, with their head held high and back straight. Now picture them suddenly slumping forward as if they are carrying an invisible weight on their shoulders – this is the physical manifestation of flatback syndrome. The condition can be caused by a number of underlying medical issues such as degenerative disc disease or low back pain, but regardless of its origin it creates postural abnormalities which need to be addressed through corrective exercise.
The transversus abdomini (TVA) muscle group plays an important role in providing stability for those suffering from flatback syndrome, as the muscles help support the spine and pelvic area. A weakened TVA can cause excessive curvature of the lower back, resulting in poor posture and increased risk for injury. Therefore, strengthening these muscles is essential when targeting treatment for patients experiencing flatback syndrome.
Corrective exercises should focus on increasing core strength while helping correct any muscular imbalances that may have contributed to the development of the condition. This may include exercises like planks, bird dogs, and hip bridges which require minimal equipment and provide maximum benefit for individuals affected by flatback syndrome. It’s also important to ensure proper form during each exercise so that targeted areas receive adequate stimulation without further straining other parts of the body.
Properly managed with corrective exercise and careful monitoring of symptoms, people experiencing flatback syndrome can significantly reduce levels of discomfort associated with their condition over time. With proper instruction from experienced physical therapists or physiotherapists, those living with flatback syndrome can take proactive steps toward improving quality of life through strengthening key muscles groups responsible for supporting spinal alignment along with improved overall posture.
Effects On The Spine
The effects of flat back syndrome on the spine can be far-reaching. This condition affects the spinal cord, which is responsible for sending signals throughout the body and also helps to maintain good posture. As a result, individuals with this disorder may experience lower back pain, neck pain, difficulty standing upright or walking, and an overall lack of mobility. In severe cases, it could lead to deformities in the spine such as scoliosis or kyphosis.
If left untreated, flat back syndrome can cause significant damage to the spine over time due to pressure being placed on vertebrae and other parts of the skeletal system. It’s essential that those who suffer from this condition seek treatment right away so they can prevent further damage and reduce their risk of requiring surgery.
At its core, treating flat back syndrome involves correcting any misalignment in the spinal curvature by strengthening underlying muscles and improving flexibility through physical therapy exercises designed specifically for this purpose. These exercises are often focused around stretching out tight muscles while simultaneously engaging weaker ones in order to restore balance within the body. With consistent effort over time, patients should notice improved stability and range of motion in their lower backs as well as their necks – two areas commonly affected by this condition.
Diagnostic Techniques
When diagnosing flat back syndrome, physical therapists typically use a combination of tests. A CT scan is often used to identify any structural abnormalities in the spine that may be causing the condition. The therapist will also conduct an extensive examination of the patient’s posture and range of motion. Physical therapy can then help determine which treatment options are appropriate for a particular case.
At a specialized spine center, further diagnostic testing such as MRI or X-ray imaging may be recommended if necessary. This additional information helps medical professionals understand the exact cause of symptoms and develop an effective treatment plan. In addition, nerve conduction studies may also be conducted to evaluate how well nerves are functioning throughout the body.
In assessing patients with flat back syndrome, physical therapists use these tools along with their own clinical knowledge to create an individualized approach for each person’s unique needs. The goal is always to restore normal function while preventing future occurrences of this painful condition.
Treatment Options
When it comes to the treatment of flat back syndrome, there is a range of options from which physical therapists can choose. It’s like having an extensive toolbox full of possible solutions that can be tailored to individual needs. These treatments often focus on pain relief, chiropractic adjustments, core muscle strengthening and stabilization exercises, or even spinal surgery if necessary.
Chiropractic adjustments are commonly used to reduce discomfort in patients with flat back syndrome by correcting any misalignment in the vertebrae or joints. This technique may also improve flexibility and increase mobility when done regularly. Core muscles should also be strengthened through various exercise programs designed specifically for this condition. Strengthening these muscles helps reduce the risk of further injury while improving posture and reducing anterior pelvic tilt associated with this disorder.
Finally, more invasive techniques such as spinal surgery may be recommended depending on severity of symptoms and how non-surgical treatments have responded so far. In some cases, surgical intervention can provide lasting relief for those suffering from severe chronic pain due to underlying disc problems that cannot be effectively treated using other methods. Ultimately, each patient must decide what route is best suited for them based on their own circumstances and preferences.
Lifestyle Modifications
The management of flat back syndrome requires a comprehensive approach which includes lifestyle modifications. Changes to daily activities can reduce the symptoms associated with this condition and prevent further injury or aggravation of the lower back pain.
To begin, it is important for individuals suffering from flat back syndrome to strengthen their core muscles, including those surrounding the vertebral column. Core muscle strengthening exercises are designed to improve posture, stabilize the spine and maintain proper alignment during movement. Additionally, abdominal muscles should be strengthened in order to support the erector spinae and other stabilizing structures throughout the torso. Regularly performing these exercises will help alleviate pain while also helping to protect against future episodes of discomfort or injury.
Finally, maintaining good flexibility through stretching can assist with reducing tightness in muscles that may be contributing to any postural dysfunction caused by flat back syndrome. As such, regular stretching sessions are strongly recommended both before and after physical activity as well as at rest periods throughout the day. Stretching helps increase range of motion while improving blood flow throughout affected areas – promoting healing and overall wellbeing.
It is essential that an individual suffering from flat back syndrome takes time each day to focus on their musculoskeletal health through appropriate exercise regimens and healthy lifestyle choices that promote proper form and function within their body’s system of joints, bones and soft tissues. By doing so they will find relief from current levels of pain while preventing further episodes down the road.
Herbal Remedies
Herbal remedies can provide relief from the chronic pain and discomfort associated with flat back syndrome. This form of natural healing has been used for centuries to treat ailments and improve physical health. To help manage symptoms, a patient may consider these four key herbal remedies:
- St Johns Wort: Used to reduce anxiety and depression which are often linked to chronic lower back pain.
- Turmeric: An anti-inflammatory that helps relieve tension in the muscles surrounding the spine and aids in spinal alignment.
- Willow Bark Extract: This contains salicin, a compound similar to aspirin, which is considered an effective pain reliever.
- Ginger Root: Considered an analgesic, it works by blocking enzymes responsible for causing inflammation throughout the body.
When treating flat back syndrome, many patients opt for non-surgical correction methods such as exercises, chiropractic care, or massage therapy before considering medications or surgical options. Herbal remedies offer another option for those looking to find relief without having to resort to taking prescription drugs or undergoing surgery. However, it’s important to consult with a qualified medical professional before beginning any treatment plan involving herbal treatments as some herbs can interact negatively with other medications or conditions you may have. With proper guidance and direction, incorporating herbal remedies into your treatment plan could be the perfect solution for managing symptoms of flat back syndrome while avoiding more invasive approaches like medication and surgery.
Over-The-Counter Medications
After discussing herbal remedies, let’s now take a look at the over-the-counter medications available to help treat flat back syndrome. Although these medications are not as effective as surgical correction, they may still provide relief from some of the symptoms associated with this condition.
First off, there are many types of pain relievers and anti-inflammatory drugs that can be used to reduce swelling in the affected area and alleviate discomfort. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen sodium can be particularly useful for cases involving chronic neck or lower back pain caused by flat back posture. Additionally, topical creams containing capsaicin or menthol can also provide temporary relief from muscle spasms in the cervical spine region.
For those suffering from more severe forms of flat back syndrome who require an orthopedic surgeon’s care, corticosteroid injections may be administered directly into the affected soft tissue to reduce inflammation and relieve pain. This type of treatment should only be done under medical supervision since it carries certain risks such as infection and adverse effects on nearby organs or tissues.
It is important to note that while over-the-counter medications can offer short-term relief from certain symptoms related to flat back syndrome, they cannot address its underlying cause nor do they replace professional medical advice. As such, individuals experiencing persistent discomfort due to this condition should seek consultation with a qualified physician for a proper diagnosis and treatment plan tailored to their specific needs.
Prescription Drugs
Are there any medications that can be used to treat flat back syndrome? Orthopedic surgeons may prescribe medication in order to reduce pain and inflammation associated with the condition. However, this is usually only done when other treatments have been unsuccessful.
Below are a few common medications prescribed for flatback syndrome:
| Medication | Use |
|---|---|
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | Reduce swelling and pain caused by inflammation. |
| Muscle relaxers | Help relieve tension, stiffness, and spasms of muscles around the spine. |
| Narcotics or opioids | Used short-term as they can become habit forming if taken long term. They help block pain signals between the brain and the body. |
Although prescription drugs can provide temporary relief from symptoms of flatback syndrome, physical therapy combined with exercise is often more effective in relieving symptoms long-term. Physical therapists will work together with patients to create an individualized plan tailored to their needs which includes strengthening exercises specifically targeted at decreasing tension on affected areas of the spine as well as improving posture. This combination has proven successful not just for symptom relief but also prevention of further injury related to flatback syndrome.
Natural Hormonal Therapy
Now that we have discussed prescription drugs for treating flat back syndrome, let’s explore an alternative therapy: natural hormonal therapy. Natural hormones are available in the form of dietary supplements and can help restore balance to your body’s own delicate hormone system. A thorough diagnosis is necessary prior to beginning any natural hormonal treatment plan, as it can be difficult to discern which hormones are out of balance without testing.
Once a diagnosis is complete, tailored exercises may be prescribed depending on what imbalances were identified during the diagnostic process. Commonly recommended exercises include core strengthening activities such as crunches and leg lifts, stretches like yoga poses or cobra pose, and aerobic activities such as walking or swimming. It is important to note that these suggested remedies should only be performed under the supervision of a certified physiotherapist who specializes in diagnosing and treating flat back syndrome.
By combining a detailed physical examination with natural hormonal therapy and tailored exercise plans, patients can experience improved posture, increased flexibility and range of motion, better pain management, and overall increased quality of life. Through this combination approach to treatment, those suffering from flat back syndrome can find relief from their symptoms and gain greater control over their condition.
Surgical Intervention
When it comes to treating flat back syndrome, surgery is often the last resort for many patients. Unfortunately, this can be a very difficult and painful process that requires lengthy recovery periods before individuals can resume their normal activities.
Take the case of one patient I worked with who experienced severe pain due to her condition. After months of physical therapy and medications failed to relieve her discomfort, she had no other choice but to undergo surgery. The procedure was successful in correcting her posture, but it took many weeks before she could begin returning to her regular daily routines. It was a long and challenging journey for both us – as we worked together towards helping her achieve better results – and my patient herself.
It’s important to remember that surgical intervention should only be considered when all other treatment options have been tried first. Surgery carries significant risks, so always seek out professional advice from your doctor or physiotherapist prior to making any decisions about treatment plans. Ultimately, you want to ensure that whatever course of action you take will provide the best possible outcome for your individual situation.
Core Strengthening Exercises
Once the diagnosis of flat back syndrome is confirmed, core strengthening exercises should be prescribed in order to improve stability and comfort. These exercises can help restore normal spinal alignment and reduce pain associated with this condition.
The core muscles are a group of muscles located around the trunk that assist in providing dynamic stability for movement. Strengthening these muscles helps to support the spine and maintain good posture during activities such as sitting or standing. Core strengthening exercises include planks, bridges, side-planks, abdominal crunches, bird dogs and squats.
For best results from core strengthening exercises it’s important to perform them correctly with proper technique and form. To ensure correct performance patients should consult with their physical therapist who will provide guidance on how to properly execute each exercise while also helping reduce any potential risk of injury due to incorrect form. When done appropriately core strengthening exercises can help build strength in the abdominals which may improve overall posture and help prevent recurrence of flat back syndrome symptoms.
Posture Correction Exercises
It is commonly thought that postural correction exercises can help manage the symptoms of flat back syndrome; however, recent research has cast some doubt on this theory. While not definitively proven to be effective, there are some simple exercises which may improve posture and reduce pain associated with flat back syndrome.
Firstly, standing wall press ups can strengthen the core muscles without putting pressure on the spine in a bent position. With feet shoulder-width apart and arms outstretched at shoulder height against a wall, slowly bend your elbows until they reach 90 degrees then straighten again for 10 repetitions. These should ideally be done twice daily for best results.
The second exercise involves using an exercise ball or seat cushion to roll up the body from head to toe while lying face up on the floor. This movement helps stretch the spine into its natural curve and strengthens abdominal muscles as well as releasing tension in tight hip flexors. Rolling up and down five times per session should suffice but can be increased over time if necessary.
Finally, it is important to keep good posture throughout everyday activities such as sitting at work or driving a car by ensuring shoulders stay relaxed and back is kept upright – poor posture could actually worsen existing problems related to flat back syndrome. Practicing these exercises regularly along with maintaining healthy lifestyle habits will contribute towards improved spinal health and overall wellbeing.
Pain Relief Strategies
Physical therapists and physiotherapists experienced in treating flat back syndrome recommend a variety of pain relief strategies. The first step is to reduce inflammation, which can be done through rest and the application of cold packs for 15 minutes at a time. Physical activity should also be limited until the symptoms subside.
In addition to reducing inflammation, physical therapy interventions such as stretching and strengthening exercises are essential components of treatment to strengthen weakened muscles and improve posture. Therapeutic massage may also provide temporary relief from muscle tension, while core stabilization exercises help to retrain abdominal muscles that have been affected by this condition. Heat application can also aid in relieving discomfort caused by tight or sore muscles.
These treatments must be tailored to each individual’s needs; what works for one person might not work for another. Patients should always communicate any changes in their levels of pain with their physical therapist or physiotherapist so that adjustments can be made accordingly. By following these guidelines, individuals will be better equipped to manage their condition and find long-term relief from chronic pain associated with flat back syndrome.
Long-Term Health Implications
Flat back syndrome can have serious long-term implications on a person’s health and quality of life, as it often leads to chronic pain in the lower back. Studies suggest that those with flat back syndrome are more prone to developing osteoarthritis or other degenerative conditions later in life due to the improper alignment of their spine. This puts them at increased risk for further disability and limitation of mobility.
It is essential that patients receive proper diagnosis and treatment from an experienced physical therapist or physiotherapist in order to minimize any possible damage caused by flat back syndrome. Through prescribed exercises targeting core muscles, gluteal muscles, hip flexors, quadriceps, hamstrings and adductors, individuals will be able to restore balance and stability to their spine while supporting its natural curvature. A combination of stretching, strengthening and postural awareness helps reduce pressure on the vertebrae over time.
Through working with a trained professional who understands the causes and effects of this condition, patients can regain control over their bodies and improve their overall well-being. Regular exercise can help alleviate symptoms associated with flat back syndrome such as stiffness, soreness, tingling sensations in limbs, limited range of motion etc., allowing individuals to reclaim their independence once again.
Conclusion
In conclusion, flat back syndrome can be a difficult condition to diagnose and manage. It is important for patients with this condition to seek out medical help from an experienced physical therapist or physiotherapist who understands the diagnosis and treatment of flatback syndrome. With my experience in treating this type of disorder, I have seen many positive outcomes from proper management.
While there may be some hesitancy on the part of patients to embark on such a journey, it is important to remember that taking action now will yield better long-term health implications than ignoring the issue. The combination of core strengthening exercises, posture correction exercises, pain relief strategies, and other treatments prescribed by your physician can help improve your quality of life and reduce discomfort associated with the condition.
At times the road ahead may seem daunting but rest assured that you are not alone in your struggle with flat back syndrome. By finding a supportive team of healthcare professionals who understand what you are going through and provide consistent effort to adhere to their plan of care, you can find success in managing this challenging disorder.